The PHE is Ending: Do You Know Where Your Waivers Are?
While the pandemic is not over, the COVID-19 public health emergency (PHE) is expected to expire soon, which means that a number of operational, safety, and billing standards that were waived at the beginning of the pandemic will be revoked. Now is the best time for providers to prepare for post-pandemic industry standards.
1. Waivers & Flexibilities Will End
Post-PHE operations will lack many of the waivers and flexibilties providers have grow accustmed to during the pandemic.
The pandemic changed how health care was administered, and for some, this change was positive. Telehealth saw a 4.6 percent increase in utilization and allowed providers to reach vulnerable populations. Responding to increased need and utilization, HHS has proposed to permanently allow behavioral health services to be furnished through audio-only technology. But not all waivers will become permanent.
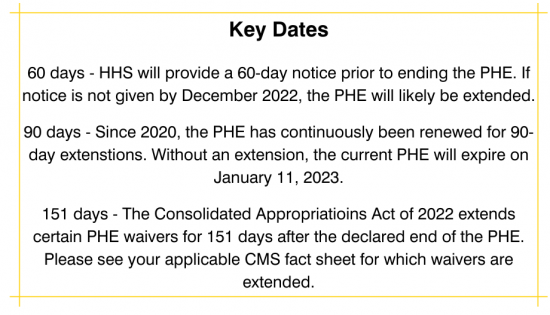
CMS has made clear that while waivers have provided healthcare providers with flexibility to respond to COVID-19, many waivers will end with the PHE. For example, telehealth flexibilities such as removing geographic or originating site restrictions and waivers expanding the types of providers able to furnish telehealth, are currently expected to expire 151 days after the declared end of the PHE. To avoid fraud violations, providers will need to be prepared to adapt their practices.
2. Fraud & Abuse Enforcement is Ramping Up
Enforcement activity is increasing. Telehealth violations, for example, appear to be a specific target. HHS-OIG recently issued a Special Fraud Alert on telemedicine activities to aid practitioners in recognizing fraud and abuse risks, while DOJ and CMS have brought criminal and administrative actions against providers involved in fraudulent telemedicine schemes. These investigations have focused on current telemedicine practices, but the increased attention should be a wake-up call to providers. Taking steps now to prepare to transition post-pandemic standards will help providers avoid fraud and abuse investigations in the future. Additionally, providers should pay attention to any state waivers that either ended with expiration of their state’s PHE or will end soon.
3. CMS has Provided Guidance for Post-PHE Operations
CMS has created helpful fact sheets organized by 16 provider-types (e.g., physicians, hospitals, home health agencies, long term care facilities) that outline the status of COVID-related Medicare waivers and flexibilities. Many waivers will end with the PHE, but legislative or administrative action could extend such waivers. Providers and institutions should review their specific CMS fact sheet for additional guidance. Fact sheets can be found here. Below are some highlights for several types of providers.
Physicians
● Remote Patient Monitoring. During the PHE, CMS permitted clinicians to bill for remote patient monitoring (RPM) for both new and established patients. But once the PHE ends, clinicians will need an established relationship with a patient before they can provide RPM services.
● Frequency Limitations. Frequency limitations for subsequent telehealth visits are returning. After the PHE, subsequent telehealth visits can only be once every three days, subsequent skilled nursing facility telehealth visits can only be once every fourteen days, and critical care consult codes furnished vie telehealth are again limited to once per day.
● Provider Enrollment. Practitioners will be required to report their home address if they are providing telehealth services from their home. Additionally, CMS is reinstating previous opt-out procedures and practitioners will not be able to cancel their opt-out status earlier than regulations allow.
Hospitals
● Telehealth Originating Site Facility Fee. At the end of the PHE, hospitals will not be able to bill a telehealth service provided at the patient’s home as if the service was provided at the hospital.
● Temporary Expansion Sites. The urgent need to increase capacity to care for the surge in patients caused CMS to waive requirements and allow for temporary expansion sites. Once the PHE ends, hospitals will be required to treat patients within their hospital facilities.
● Teaching Hospitals. Teaching physicians will once again be required to be physically present for the key portion of services furnished by a resident. But teaching physicians in remote residency training sites may still use audio/real-time communication to meet the key portion requirement, so long as the service is not surgical, high-risk, interventional, etc.
Home Health Agencies
● Clinical Records. During the PHE, CMS allowed HHAs ten business days to provide a patient a copy of their medical record. This waiver will end with the PHE and HHAs will be required to provide the record during the next visit or within four business days.
● Occupational Therapists. CMS waived previous requirements to allow OTs to perform the initial and comprehensive assessment for all patients regardless of whether occupational therapy is the service that established the patient’s eligibility. This waiver will end with the PHE.
● Training and Assessment of Aids. Currently, CMS has postponed onsite assessments to no later than 60 days after the expiration of the PHE. Following the expiration, a registered nurse will be required to make an annual onsite supervisory visit for each aid of the agency.
Long Term Care Facilities
● Three-Day Prior Hospitalization. CMS temporarily waived the three-day prior hospitalization requirement and authorized a one-time renewed skilled nursing facility coverage without a 60-day “wellness period” for certain beneficiaries. This waiver will end with the PHE.
● Required Facility Reporting. Facilities must continue to notify residents, resident representatives, and families of residents, of the status of COVID-19 in the facility. This reporting requirement will continue beyond the current PHE, until December 31, 2024.
● Pre-Admission Screening and Annual Resident Review. During the PHE, CMS allowed facilities to suspend assessments for 30 days for new nursing home residents with a mental illness or intellectual disability. After the 30-day suspension, facilities were to administer the assessments as soon as resources became available. This waiver will end with the PHE.
Final Thoughts
While many providers are still responding to the financial and operational effects of COVID-19, preparing for post-PHE requirements now will help in the long run. Even though the PHE was extended to January 2023, providers should not wait until the last minute to undo PHE processes. HHS and CMS are committed to working with providers now (providing a 60-day notice prior to the end of the PHE and provider-specific fact sheets on ending waivers), but that does not mean providers will get a “pass” from fraud and abuse investigations following the end of the PHE. The pandemic might not be over, but healthcare providers should prepare for its end.
CMS fact sheet.
PHE declarations and extensions can be found here.












